Neurodegenerative Disease: Insights from Beth Stevens’ Research
- admin
- 0
- Posted on
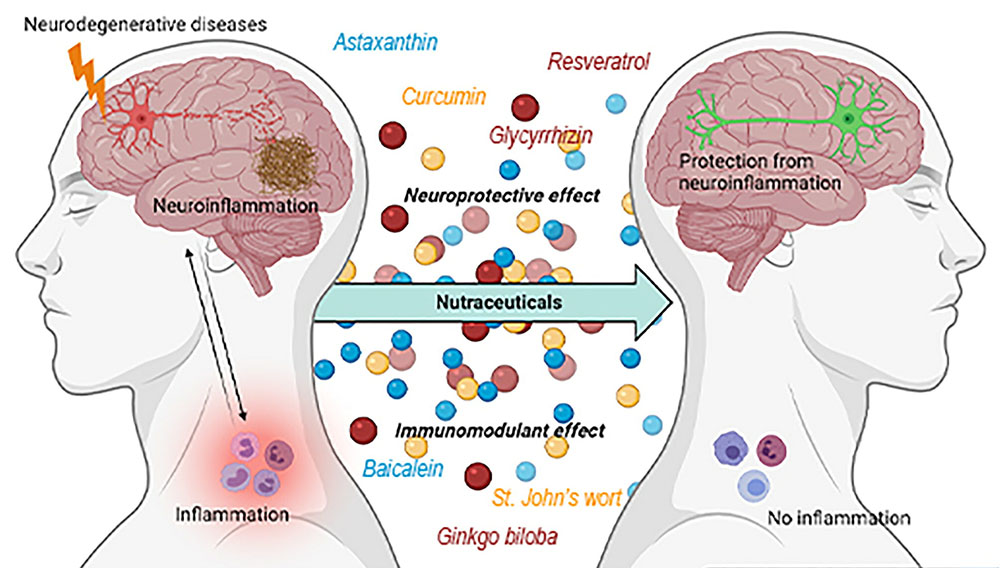
Neurodegenerative disease encompasses a range of disorders characterized by the progressive degeneration of the structure and function of the nervous system. Among these, Alzheimer’s disease stands out as one of the most prevalent conditions, affecting millions globally and emphasizing the critical need for enhanced brain health. Recent advancements in neuroscience research highlight the role of microglial cells, the immune defenders of the brain, in maintaining neuronal integrity and synaptic connections. However, when these cells malfunction, they can contribute to neurodegeneration and exacerbate conditions like Alzheimer’s and Huntington’s disease. Understanding the mechanisms behind these disruptions is essential for developing effective therapies and biomarkers aimed at alleviating the burden of neurodegenerative diseases.
The term “neurodegenerative disorder” reflects a variety of conditions where the nervous system deteriorates over time, impacting the patient’s cognitive and motor functions. Disorders like Alzheimer’s and Parkinson’s disease represent a significant public health challenge, highlighting the importance of maintaining optimal brain health. Research in neuroscience continues to uncover the functions of brain cells, including the pivotal role of microglia, in regulating neurological health. Investigating these cellular processes is crucial for unveiling the intricacies of neurodegeneration and fostering future treatments. As researchers delve deeper into these complex interactions, the quest for effective interventions becomes ever more urgent.
Understanding Microglial Cells in Brain Health
Microglial cells, often referred to as the brain’s immune guardians, play a pivotal role in maintaining brain health. These specialized glial cells are responsible for monitoring the brain’s environment, identifying threats, and clearing out debris, which is essential for optimal neurological function. Recent neuroscience research has highlighted how microglia not only remove damaged neurons but also contribute to synaptic pruning, a vital process for learning and memory formation. Their proper functioning is essential to prevent neurodegenerative diseases like Alzheimer’s, where their dysregulation can lead to increased inflammation and neuronal damage.
Beth Stevens’ transformative work has shed light on the dual role of microglial cells in both health and disease. While they are critical for synaptic maintenance and overall brain function, aberrant microglial activity has been linked to neurodegeneration. Her research indicates that when microglia misinterpret signals during neuroinflammatory responses, they may begin to excessively prune synapses, which can exacerbate conditions such as Alzheimer’s disease. By understanding these mechanisms, Stevens’ work paves the way for developing new biomarkers and therapeutic strategies aimed at restoring microglial function, ultimately enhancing brain health.
The Role of Basic Science in Neurodegenerative Disease Research
Basic science serves as the foundation for groundbreaking advancements in the field of neurodegenerative disease research. The journey of discovery often begins with seemingly unrelated studies, such as investigating the visual systems of mice, before translating into significant findings relevant to human health. Researchers like Beth Stevens emphasize that initial curiosity-driven studies are crucial for understanding complex neurobiological processes. Without this foundational knowledge, it would be impossible to make informed advancements toward treatments for diseases such as Alzheimer’s or Huntington’s.
The transformation of knowledge gained through basic research into practical applications is a gradual process, often supported by substantial federal funding from agencies like the National Institutes of Health (NIH). Stevens points out that such funding has been instrumental in her lab’s progress, allowing for sustained exploration into the role of microglial cells. It is this interplay between fundamental science and disease-specific research that creates a pathway for innovative solutions, highlighting the importance of investment in scientific curiosity as a means to combat the rising incidence of neurodegenerative diseases.
Innovations in Biomarkers for Alzheimer’s Disease
As our understanding of Alzheimer’s disease deepens, the development of new biomarkers becomes increasingly crucial for early diagnosis and treatment. Biomarkers can provide measurable indicators of disease progression, making it possible to identify Alzheimer’s in its early stages, long before cognitive decline occurs. Beth Stevens’ research on microglial cells has significant implications for this aspect of Alzheimer’s care, as her findings indicate that specific patterns of microglial activation may serve as early indicators of neurodegeneration and synaptic dysfunction.
The creation of more accurate biomarkers could revolutionize the approach to Alzheimer’s disease management, helping healthcare professionals tailor interventions more effectively. By leveraging the insights from neuroscience research regarding microglial behavior, we can develop blood tests or imaging technologies that signal pathological changes associated with Alzheimer’s. This not only aids in diagnosis but also enables monitoring the efficacy of therapeutic strategies, thereby improving brain health outcomes for millions living with this challenging condition.
Synaptic Pruning and Neurodegeneration
Synaptic pruning is a critical process that ensures the brain’s neural networks remain efficient and adaptable throughout life. However, when this process goes awry—a situation often exacerbated by neuroinflammatory conditions—it can lead to neurodegenerative diseases such as Alzheimer’s. Recent studies led by Beth Stevens emphasize the connection between improper microglial activity and aberrant synaptic pruning, suggesting that these immune cells may mistakenly eliminate healthy synapses along with damaged ones, thereby accelerating cognitive decline. Understanding this relationship is essential for developing strategies to preserve synaptic integrity in vulnerable populations.
Moreover, targeting the pathways responsible for regulating synaptic pruning could open new avenues for therapeutic intervention. By modulating microglial activity, scientists hope to restore balance within the brain, promoting healthier synaptic architectures that can fend off the effects of neurodegeneration. This innovative approach not only underscores the importance of basic science in revealing the complexities of neuronal health but also exemplifies how neuroscience research can directly inform clinical practices aimed at treating and preventing diseases like Alzheimer’s.
Future Perspectives on Treating Neurodegenerative Diseases
The future of treating neurodegenerative diseases hinges on the ongoing advancements in our understanding of brain cellular dynamics, particularly through the lens of microglial research. Beth Stevens’ work showcases how a greater comprehension of the brain’s immune functions can lead to novel therapeutic approaches aimed at curtailing diseases like Alzheimer’s. As research continues to unveil the complexities of how microglia interact with neurons, there lies unprecedented potential to develop targeted interventions that can modify disease progression.
Research collaborations are also anticipated to drive future innovations, as interdisciplinary approaches bring together expertise in neurobiology, immunology, and therapeutics. Enhanced communication across these fields can foster a more holistic understanding of how neurodegenerative diseases operate and pave the way for the development of combination therapies. By bridging gaps between basic science and clinical application, the goal of creating effective treatments for conditions like Alzheimer’s disease becomes ever more attainable.
The Impact of Funding on Alzheimer’s Research
Funding plays a crucial role in the advancement of Alzheimer’s disease research, as exemplified by Beth Stevens’ reliance on grants from the National Institutes of Health (NIH). These funds not only facilitate laboratory operations but also encourage innovative explorations that might otherwise be neglected due to financial constraints. Sustained investment in neuroscience research has the potential to lead to significant breakthroughs in understanding the mechanisms behind microglial dysfunction and neurodegeneration, providing vital insights for developing effective treatments.
In light of the rising incidence of Alzheimer’s disease, adequate funding becomes a pressing necessity. Increased financial support can help propel more studies into the mechanisms of neuroinflammation and synaptic pruning, which are crucial targets for future therapies. Moreover, establishing public-private partnerships can enhance resource availability and foster collaborative research efforts, ultimately aiming for improved outcomes for individuals affected by Alzheimer’s and contributing to the broader goal of preserving brain health across populations.
How Microglial Dysfunction Contributes to Alzheimer’s Disease
Microglial dysfunction is a significant factor in the pathogenesis of Alzheimer’s disease, leading to increased neuroinflammation that can exacerbate neurodegenerative processes. Studies reveal that when these immune cells become overly activated or fail to clear cellular debris appropriately, they can promote synaptic pruning beyond normal levels, causing further neuronal damage. Research conducted by Beth Stevens emphasizes the critical role of microglial behavior in Alzheimer’s, highlighting specific inflammatory markers that could serve as targets for intervention.
Understanding how microglial dysfunction leads to the progression of Alzheimer’s provides a pathway for developing new treatments that can mitigate inflammation and restore synaptic health. By focusing on modulating microglial activity to promote a balanced immune response, scientists aim to decrease the harmful effects associated with neurodegeneration. This approach represents a shift in therapeutic strategies, moving from symptomatic treatment to addressing underlying cellular dysfunction, which is essential for long-term management of Alzheimer’s disease.
Enhancing Public Awareness of Neurodegenerative Diseases
Raising public awareness of neurodegenerative diseases, particularly Alzheimer’s, is vital for fostering an informed community that can advocate for research funding and support affected families. Educational initiatives that highlight the role of microglial cells and their impact on brain health can empower individuals to engage with scientific developments. As prominent scientists like Beth Stevens share their findings, public discourse surrounding brain health can shift, emphasizing the importance of neurological research in combating conditions that affect millions.
Moreover, promoting awareness can facilitate early diagnosis and intervention, critical factors in managing diseases like Alzheimer’s. Families equipped with knowledge about symptoms and the importance of seeking help can lead to earlier detection, potentially slowing disease progression. Public campaigns that clarify the science behind neurodegenerative diseases can help demystify these conditions, encourage healthier lifestyle choices, and enhance overall brain health.
Navigating the Challenges of Alzheimer’s Disease Care
Caring for individuals with Alzheimer’s disease presents numerous challenges that require not only medical intervention but also emotional and logistical support. Families navigating the complexities of Alzheimer’s often face decisions regarding care options, financial implications, and the emotional toll of caregiving. Increased understanding of the disease’s mechanisms, as explained through ongoing neuroscience research, can empower caregivers with the knowledge needed to make informed choices about treatment and care.
Furthermore, community support groups and resources centered around Alzheimer’s can provide caregivers with essential tools to cope with the demands of caregiving. As researchers like Beth Stevens make strides in understanding the biological underpinnings of the disease, there is hope that these discoveries will ultimately translate into better care strategies and support systems. Addressing the holistic needs of Alzheimer’s patients is crucial for improving their quality of life and ensuring that caregivers have the resources to maintain their own well-being.
Frequently Asked Questions
What role do microglial cells play in neurodegenerative diseases like Alzheimer’s?
Microglial cells act as the brain’s immune system, crucially involved in monitoring health and responding to injury. In neurodegenerative diseases like Alzheimer’s disease, abnormal microglial activity can lead to excessive pruning of synapses, contributing to neuronal loss and disease progression.
How is neuroscience research advancing our understanding of Alzheimer’s disease?
Neuroscience research is pivotal in uncovering the mechanisms behind neurodegenerative diseases such as Alzheimer’s. Research into microglial cells has revealed their dual role in protecting brain health and potentially harming it through excessive synaptic pruning, helping to identify new therapeutic targets.
What are the recent discoveries about microglial cells in relation to Alzheimer’s disease?
Recent discoveries indicate that microglial cells not only clean up damaged neurons but also influence synaptic pruning processes that can become dysregulated in Alzheimer’s disease. These findings have implications for developing biomarkers and treatments, marking a significant step forward in combating neurodegeneration.
How can protecting brain health impact the progression of neurodegenerative diseases?
Protecting brain health is essential in slowing the progression of neurodegenerative diseases like Alzheimer’s disease. Interventions targeting inflammation and supporting microglial functions may enhance brain resilience, ultimately promoting better outcomes for affected individuals.
What is the significance of learning from basic science in addressing neurodegenerative diseases?
Basic science lays the foundation for understanding complex systems like the brain. Discovery-driven studies on microglial cells have led to significant advances in our understanding of neurodegenerative diseases, enabling the development of targeted treatments and improving patient care.
What is neurodegeneration, and how does it relate to Alzheimer’s disease?
Neurodegeneration refers to the progressive loss of neuronal structure and function, often leading to cognitive decline. Alzheimer’s disease is a leading cause of neurodegeneration, characterized by synaptic loss, neuroinflammation involving microglial cells, and the accumulation of toxic proteins in the brain.
How do biomarkers relate to neurodegenerative diseases?
Biomarkers are biological indicators that provide insight into the state of neurodegenerative diseases like Alzheimer’s. Research focused on microglial cell activity can lead to the identification of specific biomarkers that help in early detection, diagnosis, and monitoring of disease progression.
| Key Aspect | Details |
|---|---|
| Research Focus | Impact of microglial cells on neurodegenerative diseases, particularly Alzheimer’s. |
| Role of Microglia | Microglia act as the brain’s immune system, clearing out dead cells and pruning synapses. |
| Research Outcomes | Discovery of aberrant pruning links to diseases like Alzheimer’s, Huntington’s, and others. |
| Funding Support | NIH and federal funding have been crucial in advancing research. |
| Broader Implications | Research on microglial functions potentially leads to new biomarkers and treatments for neurodegenerative diseases. |
Summary
Neurodegenerative disease poses a significant challenge to healthcare, affecting millions of individuals worldwide, particularly those with Alzheimer’s disease. The groundbreaking research conducted by Beth Stevens at Harvard highlights the critical role of microglial cells in maintaining brain health and homeostasis. Her work not only sheds light on the mechanisms underlying these diseases but also sets the stage for developing innovative treatments. By understanding how microglial cells function in various conditions, researchers can pave the way to more effective interventions, thereby improving the quality of life for those affected by neurodegenerative disorders.