AI Tool Predicting Child Brain Cancer Relapse for Better Care
- admin
- 0
- Posted on
The AI tool predicting child brain cancer relapse represents a groundbreaking advancement in pediatric oncology, offering hope where traditional methods have fallen short. A recent study revealed that this innovative brain cancer prediction tool can accurately assess the risk of relapse in children diagnosed with gliomas, a type of brain tumor. By leveraging the power of temporal learning in AI, researchers have trained the model to analyze multiple brain scans over time, resulting in precision that outshines conventional approaches. This significant breakthrough aims to reduce the stress on families and improve care for young patients, ultimately changing the landscape of pediatric glioma research. As healthcare evolves through technology, the implications of this AI tool stretch far beyond mere prediction, potentially revolutionizing treatment strategies for the future.
This cutting-edge prediction system for pediatric brain cancer relapse highlights the potential of artificial intelligence in the realm of child health. The use of a sophisticated algorithm capable of analyzing serial brain scans places emphasis on the importance of comprehensive imaging data in determining glioma recurrence rates. By utilizing advanced techniques like temporal learning, the researchers have paved the way for more informed and timely decisions in managing pediatric tumors. As medical professionals seek innovative solutions, such a brain cancer prediction tool stands at the forefront of improving patient outcomes and reducing the burden of lengthy follow-up procedures. The collaboration between leading medical institutions showcases a commitment to enhancing pediatric health through intelligent technology.
Revolutionizing Pediatric Oncology with AI Tools
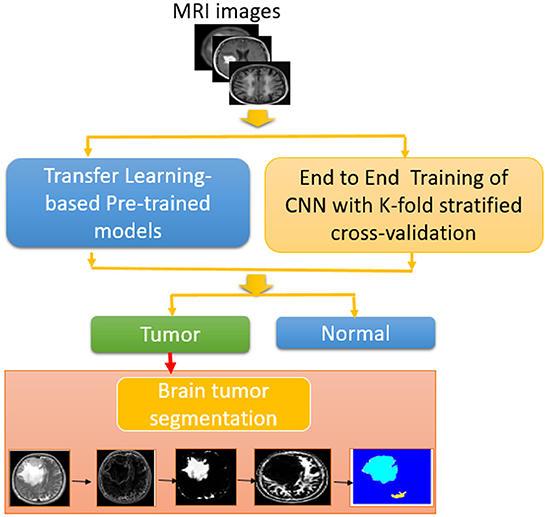
The application of AI in pediatric oncology has taken significant strides, especially in predicting outcomes for children diagnosed with brain tumors. Traditional methods of tracking the recurrence of brain cancer, specifically gliomas, rely heavily on the analysis of single time-point scans which often lead to ambiguous results. The introduction of AI tools, particularly those trained on temporal learning techniques, represents a paradigm shift. By synthesizing data from multiple brain scans acquired over time, these models provide a more comprehensive understanding of how a tumor evolves, drastically improving prediction accuracy.
Mass General Brigham’s groundbreaking research highlights this very innovation, showcasing an AI tool capable of analyzing nearly 4,000 MR scans to predict relapse risk in pediatric glioma patients. These advanced brain cancer prediction tools not only enhance the precision of prognostic assessments but also contribute to the overarching goal of personalized medicine. By tailoring monitoring strategies based on the identified risk levels, healthcare providers can optimize care pathways, ultimately reducing the emotional and physical burden on young patients and their families.
The Impact of Temporal Learning in AI for Brain Cancer Prediction
Temporal learning, as applied in recent studies, stands as a cornerstone of innovative approaches to predictive modeling in pediatric glioma research. Unlike traditional AI models that focus on individual scans, temporal learning incorporates a sequence of images collected over months. This method allows the AI to recognize minor evolutions in tumor characteristics that might signify potential relapse, leveraging historical data to enhance future predictions. By systematically analyzing sequential MR scans, patients’ risk levels can be assessed with much greater detail and accuracy.
The results from research at Mass General Brigham indicate that incorporating multiple timepoints enhances the predictive capability of AI tools significantly. With accuracies soaring to figures between 75-89 percent for identifying glioma recurrence within a year post-treatment, the benefits are clear. Distinguishing between low- and high-grade gliomas becomes more feasible, allowing for stratified treatment plans. This nuanced understanding aims to mitigate unnecessary imaging for patients with lower risk while ensuring that those identified as high-risk receive timely, targeted adjuvant therapies.
Improving Care for Pediatric Glioma Patients
The goal of advanced AI predictions in pediatric glioma cases is more than just tracking disease progression; it is about enhancing overall care quality for children battling brain cancer. The study from Mass General Brigham emphasizes the potential for AI tools to alter pediatric oncology techniques profoundly. By providing accurate relapse predictions, physicians can make informed decisions on the frequency of follow-up MRIs based on individual patient risk profiles, significantly relieving the emotional and physical toll that regular imaging can impose on families.
Moreover, understanding the recurrence risk earlier may prompt interventions that are timely and more tailored to patient needs. Children categorized as high-risk could benefit from proactive treatments, thereby possibly improving long-term outcomes. The emphasis on using AI to guide clinical decision-making underscores the commitment to delivering precision medicine in pediatric oncology, ensuring that every child receives the most appropriate and effective care.
The Role of Collaborations in Pediatric Cancer Research
Collaboration plays a vital role in advancing pediatric glioma research and improving patient outcomes. The recent study published in The New England Journal of Medicine AI embodies the strength of partnerships formed between institutions like Mass General Brigham, Boston Children’s Hospital, and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center. Such collaborations enable the pooling of resources, expertise, and robust datasets, which are critical for training AI models effectively.
These cooperative efforts not only enrich the research dimension but also pave the way for future clinical applications of AI tools in oncology. The potential for collecting large and diverse datasets enhances the generalizability of findings, making it easier to validate and implement these tools in various clinical settings across the nation. As collaborative pediatric glioma research continues to evolve, it is expected that further breakthroughs will emerge, significantly impacting treatment protocols and patient care strategies.
Ensuring the Future of Pediatric Cancer Care with AI
As we look to the future, the integration of AI tools in pediatric oncology seems promising, especially in predicting brain cancer relapses. The findings from Harvard’s research demonstrate a clear pathway toward enhanced risk stratification and tailored patient management. However, the call for further validation in diverse clinical settings remains crucial. The need for robust clinical trials will ensure these AI systems can transition from research environments to everyday practice, guaranteeing that they provide real-world benefits.
The commitment to utilizing advanced technologies cannot be overstated; it represents a significant leap toward automated and precise healthcare solutions. By focusing on AI’s predictive abilities, the goal of reducing unnecessary interventions while providing critical support for high-risk patients is more attainable than ever. With ongoing developments in areas like temporal learning in AI, the field is excited about the innovations that will permeate pediatric glioma treatment strategies, potentially saving countless young lives.
Challenges Ahead for AI in Pediatric Oncology
Despite the successes noted in recent AI studies, challenges remain in the integration of these advanced tools into clinical practice for pediatric oncology. One significant issue is ensuring data privacy and security, particularly when dealing with sensitive health information of minors. The deployment of AI tools must adhere to stringent ethical standards to protect patient data while maintaining the accuracy of predictions.
Another hurdle is the need for comprehensive training among healthcare professionals on how to interpret AI-generated predictions. While these tools can enhance decision-making, physicians must be equipped with the skills to understand and leverage AI insights effectively. This necessitates dedicated educational initiatives that can help bridge the gap between traditional practices and emerging technologies in pediatric glioma care.
AI’s Promise in Longitudinal Imaging and Pediatric Glioma
The innovation behind using AI tools in longitudinal imaging has great implications for the management of pediatric gliomas. By employing techniques like temporal learning, medical professionals can meticulously track tumor changes over time, which serves a dual purpose: facilitating timely medical interventions and alleviating the anxiety associated with frequent hospitalization and imaging.
As pediatric hospitals adopt more sophisticated imaging technologies alongside this AI capability, the potential for refining treatment pathways beams with optimism. Regular, detailed timelines of a child’s health status not only inform better clinical decisions but also provide families with clearer insights into their child’s prognosis, formation of a collaborative approach in care that instills trust and reassurance.
Empowerment through Predictive Analytics in Pediatric Cancer
In the evolving landscape of pediatric oncology, empowering families with information through predictive analytics stands paramount. With the advent of AI tools predicting the risk of relapse in brain cancer, parents can be more proactive in discussions about treatment plans and future care options. This shift from reactive to proactive healthcare management is instrumental in fostering a sense of agency among families at a time when they often feel helpless.
Moreover, the predictive data provided by advanced AI models can serve a dual role: not only aiding clinicians in developing personalized care plans but also enabling families to participate in decision-making processes actively. Patients and their guardians can collaborate with oncologists to weigh the implications of various treatment strategies based on predicted risks, thus creating a more tailored and supportive healthcare journey.
The Need for Comprehensive Clinical Trials in AI Applications
As promising as recent developments in AI for pediatric glioma prediction are, the transition to clinical application will necessitate comprehensive clinical trials that assess both efficacy and safety. These trials must encompass a diverse population of pediatric cancer patients to ensure that the AI models developed are effective across various demographics. Ensuring that all children have access to cutting-edge AI tools is paramount for widespread acceptance and utilization in clinical environments.
Moreover, trials should evaluate the long-term implications of AI-guided treatment strategies, looking beyond immediate outcomes to consider how these innovations affect overall quality of life for young patients. Only through rigorous testing can the pediatric oncology community confidently integrate AI tools into standard practice, paving the way for a healthier future for children battling cancer.
Frequently Asked Questions
How does the AI tool predicting child brain cancer relapse improve outcomes in pediatric glioma patients?
The AI tool designed for predicting child brain cancer relapse enhances patient outcomes by analyzing multiple brain scans over time rather than relying on single images. This temporal learning allows for a more accurate prediction of glioma recurrence, significantly improving risk assessment and enabling tailored treatment strategies.
What is the role of temporal learning in AI for glioma recurrence prediction?
Temporal learning is crucial in the AI tool predicting child brain cancer relapse as it enables the model to synthesize information from various brain scans taken over months. This innovative approach improves accuracy in predicting glioma recurrence by recognizing subtle changes in the patient’s imaging data over time.
What are the benefits of using an AI brain cancer prediction tool in pediatric oncology?
The AI brain cancer prediction tool offers numerous benefits in pediatric oncology, including enhanced accuracy in predicting relapse risks, reducing unnecessary follow-up imaging for low-risk patients, and potentially allowing for early interventions in high-risk cases, thereby improving overall care for children diagnosed with gliomas.
How accurate is the AI tool predicting child brain cancer relapse compared to traditional methods?
The AI tool predicting child brain cancer relapse has demonstrated an accuracy of 75-89% in identifying recurrence of gliomas, which is significantly higher than traditional prediction methods that yield approximately 50% accuracy. This advancement in pediatric glioma research represents a vital step toward better predictive analytics in oncology.
What data was used to train the AI tool for predicting pediatric glioma recurrence?
The AI tool for predicting pediatric glioma recurrence was trained using nearly 4,000 magnetic resonance imaging scans from 715 pediatric patients. This comprehensive dataset allowed the researchers to leverage temporal learning effectively, leading to improved accuracy in detecting brain cancer relapses.
Are clinical trials planned for the AI tool predicting child brain cancer relapse?
Yes, researchers plan to launch clinical trials to further validate the AI tool predicting child brain cancer relapse. These trials aim to determine whether AI-informed predictions can enhance care strategies, such as optimizing imaging frequency and informing treatment options for high-risk pediatric glioma patients.
What is the impact of accurate glioma recurrence prediction on treatment strategies for children?
Accurate glioma recurrence prediction through AI enhances treatment strategies for children by enabling personalized management plans. For low-risk patients, it reduces the frequency of stressful imaging sessions, while high-risk patients can benefit from timely interventions, potentially leading to better survival rates and improved quality of life.
How does the AI tool for glioma recurrence prediction differ from traditional imaging analysis?
Unlike traditional imaging analysis, which often relies on a single scan, the AI tool for glioma recurrence prediction employs temporal learning to analyze a series of scans over time. This method allows for a deeper understanding of tumor progression signals, leading to a more nuanced assessment of patient risk levels.
In what ways can AI in pediatric oncology transform the care process for brain cancer patients?
AI in pediatric oncology, particularly through tools predicting child brain cancer relapse, can transform the care process by providing more precise diagnostics, reducing unnecessary medical interventions, facilitating early treatment for at-risk children, and ultimately improving clinical outcomes and patient experiences in managing pediatric gliomas.
What challenges remain in implementing AI tools for predicting child brain cancer relapse in clinical settings?
Despite the promising results of AI tools in predicting child brain cancer relapse, challenges remain, including the need for further validation in diverse clinical settings, acceptance among healthcare providers, integration into existing workflows, and ensuring equitable access to AI-driven technologies for all pediatric patients.
| Key Points | Details |
|---|---|
| Traditional Methods Insufficient | Predicting cancer relapse risk in pediatric patients has traditionally been inaccurate. |
| AI Tool Advantage | A Harvard study shows that an AI tool predicts relapse risk with 75-89% accuracy, compared to 50% accuracy using single images. |
| Temporal Learning | The AI uses temporal learning to analyze multiple scans over time for better prediction. |
| Study Collaborators | Mass General Brigham, Boston Children’s Hospital, and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center contributed to the research. |
| Future Directions | The researchers aim to conduct clinical trials to validate AI predictions and improve patient care. |
Summary
The AI tool predicting child brain cancer relapse represents a significant advancement in pediatric oncology. Researchers have developed a method that far surpasses traditional techniques, significantly enhancing the accuracy of relapse predictions in children with gliomas. With the potential to alleviate the burden of frequent imaging on young patients and tailor treatments based on risk assessment, this innovative technology could transform how we approach the care of children with brain cancers.