U.S. Maternal Mortality Rates: A Call for Immediate Action
- admin
- 0
- Posted on
U.S. maternal mortality statistics reveal a troubling trend, as pregnancy-related deaths have continued to rise, marking the nation as a leader in maternal mortality among high-income countries. With over 80% of these deaths deemed preventable, it raises questions about the adequacy of maternal health services provided throughout pregnancy and postpartum care. The reality is stark; cardiovascular disease deaths now account for a significant portion of these fatalities, highlighting a critical intersection between chronic health conditions and pregnancy. Furthermore, the racial disparities in maternal health outcomes remain alarming, with American Indian and Alaska Native women facing the highest mortality rates. Addressing these pressing issues is crucial for improving maternal health and ensuring every pregnancy is safe and supported in the U.S.
The rising number of maternal deaths in the United States highlights a severe public health crisis, particularly in terms of maternal wellbeing during the perinatal period. This rise, characterized by a surge in complications during and after childbirth, emphasizes the urgent need for enhanced prenatal care and better postpartum support systems. Alarmingly, cardiovascular issues have emerged as the leading causes of death among new mothers, pointing to a growing trend in chronic health problems affecting pregnant individuals. Additionally, systemic inequities continue to perpetuate significant racial disparities in maternal health outcomes, revealing deep-seated issues in healthcare access and quality. To combat these challenges, comprehensive strategies and policies must be implemented to safeguard maternal health across all demographics.
The Alarming Rise of U.S. Maternal Mortality
The U.S. has long been criticized for its exceptionally high rates of maternal mortality compared to its high-income peers. As highlighted in recent studies, while over 80% of these deaths are deemed preventable, the country’s maternal mortality rates continued to rise from 2018 to 2022, marking a troubling trend. The latest statistic of approximately 32.6 deaths per 100,000 live births in 2022 signifies a call to action for health authorities and policymakers alike. This spike in pregnancy-related deaths is not only alarming but underscores the urgent need for comprehensive maternal and postpartum care that can address the varied factors contributing to this crisis.
Many believe that the fragmented healthcare system significantly contributes to the disparities in maternal health outcomes. The lack of cohesive policies, compounded by racial inequities, exacerbates the situation; American Indian and Alaska Native women face much higher pregnancy-related mortality rates than their white counterparts. It is imperative to recognize that addressing these disparities involves not only healthcare access but also a systemic overhaul to ensure that all women receive equitable care regardless of race or geographic location.
Additionally, the increase in maternal mortality rates has been attributed to various social determinants of health, including socioeconomic factors and the accessibility of quality healthcare. For instance, maternal health is heavily influenced by underlying chronic conditions, many of which are on the rise among younger populations. This shift towards cardiovascular disease as a leading cause of pregnancy-related death highlights the need for targeted interventions aimed at managing these chronic conditions more effectively within women of reproductive age, particularly in high-risk groups.
Furthermore, the COVID-19 pandemic has also played a significant role in the observed decline in maternal health outcomes, as it has strained already vulnerable healthcare systems. The challenge now lies in leveraging the lessons learned from this turbulent period to foster robust health policies that prioritize the protection of maternal health, ensuring that future generations of women do not face the same challenges.
Reducing Racial Disparities in Maternal Health
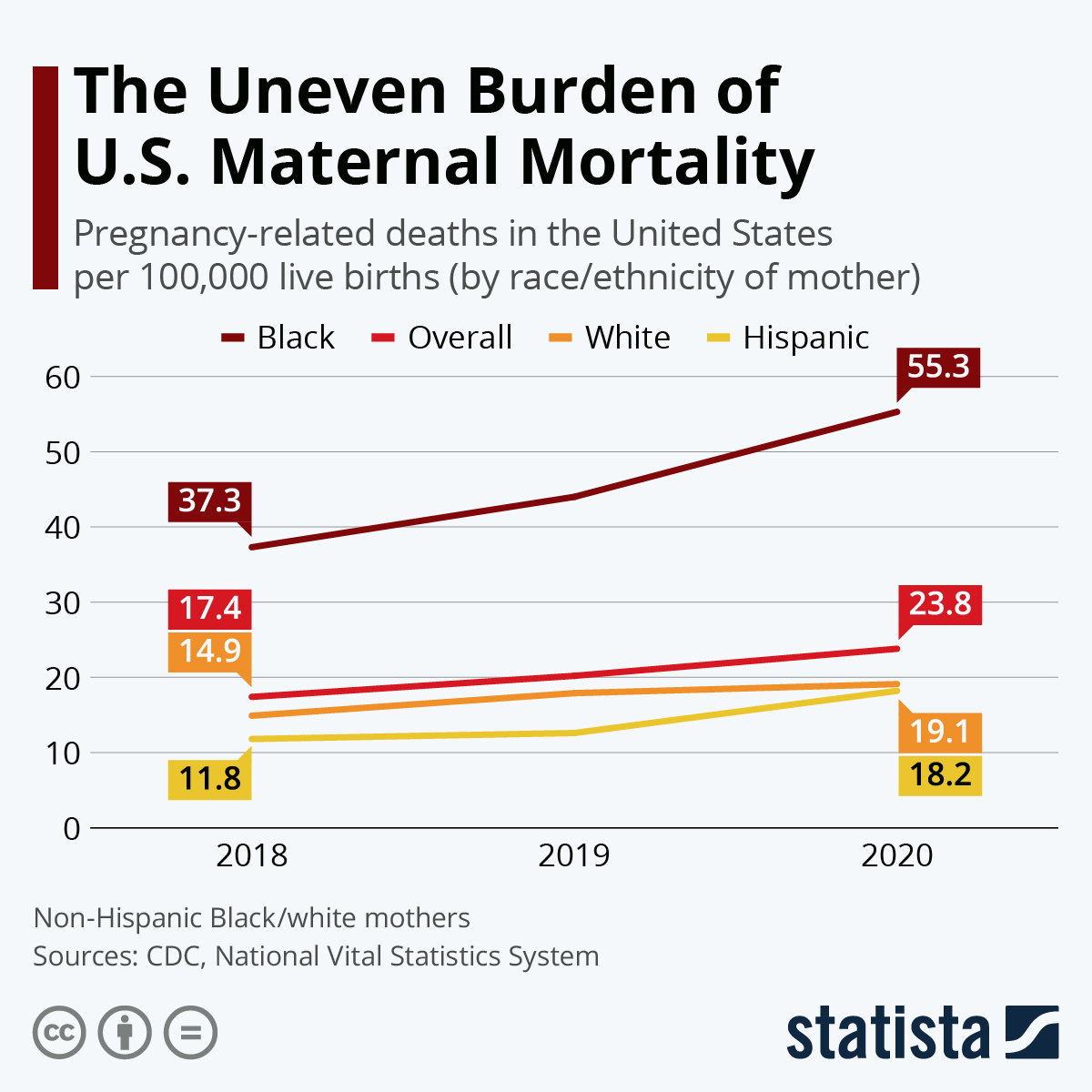
Racial disparities in maternal health outcomes have been a persistent issue in the U.S., with studies revealing disproportionate rates of pregnancy-related deaths among minority populations. For instance, non-Hispanic Black women are over three times more likely to experience maternal mortality compared to white women. This stark reality calls for immediate and sustained efforts to address systemic biases that transcend healthcare settings, impacting everything from prenatal care access to post-delivery support. These disparities also entail a comprehensive understanding of the socio-economic factors contributing to adverse health outcomes for different racial and ethnic groups.
Addressing these disparities requires a multifaceted approach, focusing on not only improving healthcare delivery but also targeting the underlying social determinants of health. For example, initiatives aimed at enhancing healthcare access in under-resourced communities are essential. This includes expanding equitable access to prenatal and postpartum care while also providing educational resources that empower women with the knowledge necessary to advocate for their health. Furthermore, involving community organizations that work closely with these demographics can lead to culturally competent care that addresses specific needs and concerns.
Innovative approaches are also emerging within the healthcare system aimed at bridging these gaps. One effective strategy is to implement maternal health advocate programs that connect vulnerable populations to appropriate healthcare services, thus improving engagement and compliance with treatment recommendations. By training advocates who understand the challenges faced by various communities, healthcare providers can foster relationships that promote trust and encourage women to seek timely care throughout their pregnancy and postpartum periods.
Moreover, addressing broader systemic issues, such as maternal health funding cuts, is crucial. As recent budgets reflect a deprioritization of maternity care, it’s essential to rally support for policies that recognize the unique challenges faced by marginalized groups. This will not only combat racial disparities but also ensure that all mothers receive the quality care they deserve, ultimately reducing the incidence of unnecessary pregnancy-related deaths.
The Role of Cardiovascular Disease in Maternal Mortality
Interestingly, cardiovascular disease has emerged as one of the leading causes of maternal mortality in the U.S., with an alarming increase noted in recent years. Factors such as chronic hypertension have become more prevalent among younger women, resulting in higher rates of complications that can contribute to pregnancy-related deaths. This shift from previously predominant causes, such as hemorrhage, highlights the evolving nature of health risks associated with pregnancy, demanding increased awareness and proactive management of cardiovascular health for maternal patients.
Healthcare providers need to prioritize screening for cardiovascular conditions among pregnant individuals, especially those with pre-existing risks or those belonging to high-risk populations. This can help in early identification and management of issues such as preeclampsia or gestational hypertension, which significantly increase the risk of maternal death. Moreover, sustained postpartum care that focuses on heart health can further mitigate risks associated with cardiovascular disease among new mothers.
Efforts to educate both patients and healthcare professionals about the signs and symptoms of cardiovascular complications during and after pregnancy are vital components in combatting this issue. Training for obstetricians and midwives on the relationship between maternal health and cardiovascular conditions, alongside integrated care models that include cardiology specialists, can pave the way for more comprehensive care plans that address this leading cause of maternal mortality effectively.
Furthermore, public health initiatives aimed at reducing cardiovascular disease risk factors before pregnancy can lead to significant improvements in maternal health outcomes. This includes promoting healthier lifestyles, providing access to preventive healthcare services, and developing community programs that target women’s heart health awareness. By taking a proactive stance on cardiovascular health, we can aim to reduce the incidence of maternal mortality linked to heart disease, ultimately safeguarding the lives of mothers and their infants.
The Importance of Postpartum Care in Maternal Health
The postpartum period, crucial to maternal recovery, is often overlooked in discussions about maternal health and mortality. Many healthcare systems traditionally focus on the immediate weeks following delivery, neglecting the importance of ongoing care in the months thereafter. Recent evidence suggests that nearly one-third of maternal deaths occur during the late postpartum period, highlighting a vital opportunity to enhance care strategies that encompass this critical timeframe, ideally extending support for up to a year after childbirth.
Late maternal deaths often are linked to chronic conditions that require ongoing management, such as hypertension and diabetes, which may go unaddressed in the absence of structured follow-up care. Implementing comprehensive postpartum care plans that include regular check-ups, mental health screenings, and education on managing chronic conditions can significantly improve maternal health outcomes and reduce mortality rates. The goal should be to ensure that new mothers receive continuous support tailored to their specific health needs.
Moreover, education is a pivotal aspect of effective postpartum care. Healthcare providers should equip postpartum patients with information regarding warning signs of complications that could arise weeks or months after delivery. This can empower women to seek help promptly and reduce the risk of preventable deaths. Integrating mental health support within postpartum care is equally essential, considering the profound impact that emotional wellbeing has on maternal health.
In conclusion, extending the focus of maternal care beyond the delivery room and into the entirety of the postpartum phase is crucial. By prioritizing and investing in comprehensive postpartum care, the healthcare system can ensure that mothers not only survive childbirth but thrive in their role as new parents, ultimately improving maternal health outcomes nationwide.
Preventing Pregnancy-Related Deaths Through Policy Change
Addressing the alarming rates of pregnancy-related deaths in the U.S. necessitates an examination of existing health policies that may inadvertently contribute to this crisis. Despite the wealth of data indicating that many maternal deaths are preventable, systemic gaps in policy and access to care persist. Advocacy for robust reforms—such as expanding Medicaid coverage to the postpartum period and improving healthcare access for vulnerable populations—are crucial in reducing the overall maternal mortality rate and addressing the disparities evident among different demographics.
This urgent call for policy reform is clear: enhancing maternal health services from prenatal care through to postpartum recovery can lead to a significant reduction in mortality rates. States that have implemented such policies, like California, provide valuable models for the nation. By identifying successful initiatives and encouraging other states to adopt similar measures, we can work towards standardizing quality care for all mothers.
As we push for improvements in policy surrounding maternal care, collaboration among healthcare providers, policymakers, and community organizations is essential. Gathering data on maternal health outcomes can inform evidence-based practices that address the unique challenges different demographics face, particularly in racially diverse communities. Public involvement and advocacy are vital in keeping maternal health as a priority within political discussions, especially in light of ongoing budget cuts that threaten the future of maternal health programs.
Ultimately, ensuring every mother has access to comprehensive, equitable care before, during, and after pregnancy should be a shared commitment across all sectors of society. By fostering supportive policies and community-driven initiatives, we can create an environment conducive to healthier pregnancies and improved maternal health outcomes.
Addressing Chronic Health Conditions to Improve Maternal Outcomes
The rising incidence of chronic health conditions among women of reproductive age is a concerning factor contributing to increased maternal mortality rates. Conditions like hypertension, diabetes, and obesity can significantly complicate pregnancies and lead to severe health implications during and after childbirth. To mitigate these risks, there is a growing imperative for healthcare systems to prioritize the management of chronic diseases before and throughout pregnancy. By identifying and addressing these conditions early, healthcare providers can better support women in achieving healthy pregnancies and improve overall maternal health outcomes.
Implementing preventive strategies such as lifestyle modifications, regular screenings, and accessible healthcare services is vital in combating the chronic disease crisis. Education surrounding the management of these conditions can empower women, helping them navigate their health effectively while pregnant. Moreover, collaborative care models that include primary care, obstetricians, and specialists can enhance treatment approaches by fostering a more integrated strategy for managing chronic diseases and supporting maternal health.
In addition to clinical management, addressing social determinants of health is crucial in reducing the prevalence of chronic conditions among women. Targeting factors such as nutrition, physical activity, and stress management through community programs can provide significant benefits for women preparing for motherhood. Whether through public health campaigns or supportive local initiatives, ensuring women have the resources they need for maintaining optimal health is paramount in reducing risks during pregnancy.
Ultimately, the healthcare framework must recognize and address the interplay between chronic health conditions and maternal outcomes. By taking holistic approaches that incorporate education, improved access to care, and lifestyle changes, we can work towards decreasing the maternal mortality rate and fostering healthier communities for future generations.
The Urgency of Comprehensive Maternal Health Research
Comprehensive research on maternal health is more pressing than ever, particularly in light of the rising maternal mortality rates across the United States. The discontinuity in tracking maternal deaths prior to 2018 has hindered our understanding of this complex issue, making it imperative that robust research initiatives are prioritized and funded appropriately. Continued studies will help identify more nuanced factors contributing to pregnancy-related deaths, including environmental influences and access to healthcare, thus allowing policymakers to create informed, targeted interventions that address the needs of diverse populations.
Furthermore, ongoing research can illuminate the systemic barriers within the healthcare system that perpetuate racial and ethnic disparities in maternal health. With a more thorough understanding of these disparities, stakeholders can challenge barriers effectively and seek to implement best practices adopted from successful healthcare models within various states and communities.
Investing in maternal health research also extends to education and training for healthcare providers, enabling them to identify risks and respond effectively to complications during pregnancy and after childbirth. Research findings should be translated into practical guidelines that inform clinical practice and foster a comprehensive understanding of maternal health issues among medical professionals.
Ultimately, the commitment to research is foundational in creating a sustainable framework for improving maternal health outcomes in the U.S. By harnessing data-driven insights to inform policy and practice, we can work toward a future where pregnancy-related deaths are significantly reduced, and mothers receive the quality care they need and deserve.
Frequently Asked Questions
What are the main factors contributing to U.S. maternal mortality rates?
U.S. maternal mortality rates are significantly influenced by a patchwork healthcare system, inequitable policies, and maternity care deserts. Additionally, persistent racial disparities in maternal health contribute to higher pregnancy-related deaths, particularly among American Indian, Alaska Native, and non-Hispanic Black women. Chronic health conditions such as cardiovascular disease have also become more prevalent among younger individuals, exacerbating these issues.
How does cardiovascular disease relate to maternal mortality in the U.S.?
Cardiovascular disease is a leading cause of pregnancy-related deaths in the U.S., accounting for over 20% of maternal deaths. The rising incidence of conditions like hypertension, pre-eclampsia, and cardiac complications during pregnancy highlights the increasing risk for women. This shift indicates that younger women are now facing these chronic health issues more frequently than in the past.
What role does postpartum care play in U.S. pregnancy-related deaths?
Postpartum care is crucial for preventing maternal mortality, as nearly a third of pregnancy-related deaths occur between 42 days and one year after delivery. Better healthcare systems should recognize the postpartum period as a continuum beyond the traditional six weeks, addressing the ongoing health needs of new mothers to reduce late maternal deaths.
Why are there racial disparities in U.S. maternal health outcomes?
Racial disparities in maternal health outcomes are rooted in systemic bias, inequitable healthcare access, and sociopolitical factors. American Indian and Alaska Native women experience the highest maternal mortality rates, nearly four times that of white women. Addressing these disparities requires targeted policy changes and improved healthcare access for marginalized communities.
What policies could help reduce U.S. maternal mortality rates?
To effectively reduce U.S. maternal mortality rates, policies should focus on expanding access to quality prenatal and postpartum care, particularly in underserved areas. Implementing comprehensive public health strategies to monitor maternal health outcomes and ensuring equitable healthcare access for all racial and ethnic groups are critical steps for improving maternal health nationwide.
How has the COVID-19 pandemic impacted U.S. maternal mortality rates?
The COVID-19 pandemic has had a significant impact on U.S. maternal mortality rates, especially noted in the sharp increase during 2021. The pandemic’s strain on healthcare systems likely exacerbated existing issues and contributed to the rising rates of pregnancy-related deaths, necessitating a critical reassessment of maternal health strategies.
What is the significance of late maternal deaths in understanding maternal mortality?
Late maternal deaths, which occur between 42 days and up to one year postpartum, represent a significant portion of pregnancy-related deaths. Recognizing this timeframe is vital for improving healthcare systems and resources dedicated to postpartum care, which traditionally have been neglected, leading to preventable fatalities.
What are the most common causes of preventable maternal deaths in the U.S.?
The most common causes of preventable maternal deaths in the U.S. include cardiovascular diseases, hemorrhage, infection, and complications related to pre-existing conditions. Addressing these issues through enhanced prenatal care and monitoring could significantly reduce pregnancy-related deaths.
How can advancements in maternal health tracking improve outcomes?
Advancements in tracking maternal health, such as the pregnancy checkbox on death certificates, provide crucial data for identifying trends and disparities in maternal mortality. This data can inform policies and interventions aimed at reducing pregnancy-related deaths and enhance the overall quality of maternal care.
What impact do socioeconomic factors have on U.S. maternal mortality rates?
Socioeconomic factors play a crucial role in U.S. maternal mortality rates as they influence access to healthcare, nutrition, and overall health conditions. Women from lower socioeconomic backgrounds often face barriers to quality care, leading to higher risks of pregnancy-related deaths.
| Key Points | Details |
|---|---|
| Rising Maternal Mortality | U.S. has the highest maternal mortality rate among high-income countries, with rates continuing to rise from 2018 to 2022. |
| Preventable Deaths | More than 80% of pregnancy-related deaths are preventable. |
| Disparities in Mortality | Significant disparities exist based on race and state; American Indian and Alaska Native women have the highest mortality rates. |
| Impact of COVID-19 | The sharpest increase in mortality rates was observed in 2021, coinciding with the COVID-19 pandemic. |
| Leading Causes of Death | Cardiovascular disease is the leading cause of pregnancy-related deaths, affecting even younger women. |
| Late Maternal Deaths | Nearly one-third of total deaths occur between 42 days and 1 year postpartum, necessitating better long-term care. |
| Need for System Changes | Investment in public health infrastructure and innovative care solutions is crucial for improving maternal health outcomes. |
Summary
U.S. maternal mortality remains a critical issue with alarming trends highlighted by recent research indicating that the rates have continued to rise in recent years. Over 80 percent of these deaths are preventable, revealing significant gaps in healthcare access and quality across different demographics. The disparities based on race and state further emphasize the urgent need for comprehensive healthcare reforms and better support systems for pregnant individuals. As the nation grapples with these challenges, it is essential to prioritize maternal health to prevent unnecessary loss of life and improve care strategies throughout pregnancy and into the postpartum phase.