TIM-3 Therapy for Alzheimer’s: A New Frontier in Treatment
- admin
- 0
- Posted on
TIM-3 therapy for Alzheimer’s is emerging as a promising new approach in the field of Alzheimer’s treatment. This innovative strategy draws insights from immune checkpoint inhibitors, which have showcased success in cancer therapies. By targeting the TIM-3 gene, researchers aim to enhance the function of microglia—brain cells that clean up amyloid plaques linked to Alzheimer’s. Recent studies indicate that inhibiting TIM-3 can free these crucial immune cells to effectively combat plaque buildup, leading to significant cognitive enhancement in animal models. As scientists delve deeper into this revolutionary method, the potential for improving memory and overall brain health in Alzheimer’s patients becomes increasingly tangible.
The exploration of TIM-3 as a therapeutic avenue for Alzheimer’s disease represents a pivotal shift in how we understand and treat cognitive decline. By leveraging immune strategy insights originally developed for malignancies, researchers are finding new ways to stimulate brain function. Specifically, the role of immune molecules, particularly those akin to TIM-3, highlights the intricate relationship between immunity and neurodegeneration. As studies unveil the protective roles of microglia against harmful plaques, they pave the way for innovative Alzheimer’s interventions that promise not just symptom management but potential reversibility. This developing landscape of treatment heralds new hope for millions affected by cognitive disorders.
The Role of TIM-3 in Alzheimer’s Disease
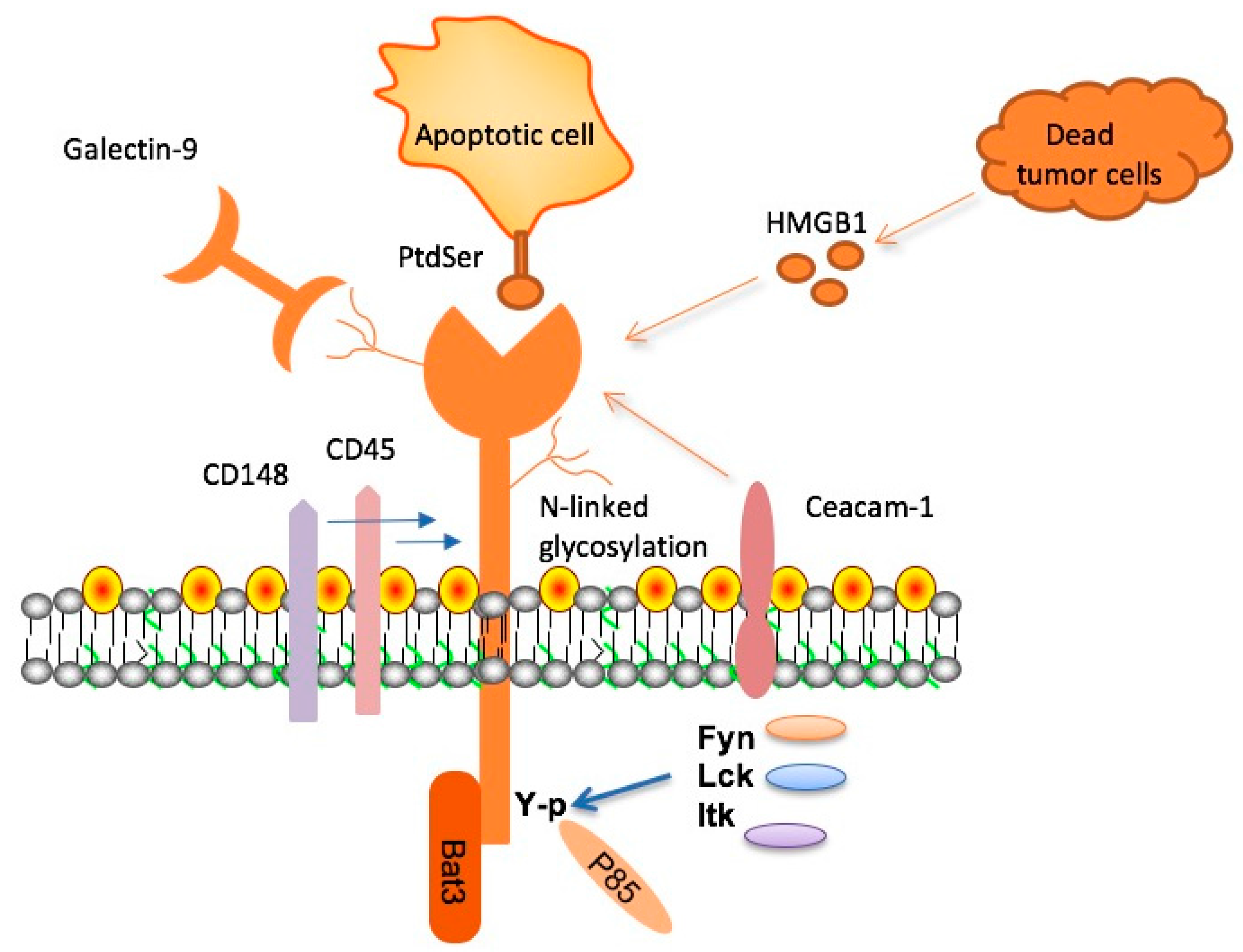
The TIM-3 molecule has emerged as a critical player in the context of Alzheimer’s disease (AD), particularly in its late-onset form, which accounts for approximately 90 to 95 percent of all cases. A significant genetic risk factor linked to AD has been identified within the TIM-3 gene, HAVCR2. This gene’s polymorphism can result in high levels of TIM-3 expression on microglial cells, inhibiting their ability to clear amyloid plaques from the brain. Essentially, while TIM-3 serves as a regulatory checkpoint to manage immune responses, its overexpression in Alzheimer’s leads to microglial dysfunction, preventing necessary phagocytosis of harmful plaques and exacerbating cognitive decline.
In healthy conditions, microglia are vital for maintaining brain health by removing waste and supporting synaptic pruning, crucial for memory preservation. However, an increase in TIM-3 interferes with this process. Rather than clearing the accumulated beta-amyloid, microglia become homeostatic and less responsive to the harmful protein aggregates, creating a detrimental cycle that contributes to AD pathology. This interplay underscores the opportunity for TIM-3 therapy for Alzheimer’s, aiming to reestablish the microglial function and enhance cognitive health by blocking or downregulating TIM-3 activity.
Understanding the dual role of TIM-3 is fundamental for developing effective Alzheimer’s treatments. Its primary function is to prevent autoimmunity by inhibiting excessive immune responses. However, in the context of Alzheimer’s disease, this inhibition leads to a failure in clearing amyloid plaques. As TIM-3 levels rise, microglial viability and their ability to prune unnecessary synapses diminish, leading to memory impairments characteristic of Alzheimer’s. This insight is key to leveraging TIM-3 therapy as a pivotal strategy in restoring cognitive function and mitigating the progression of Alzheimer’s disease.
Recent research has shown that deletion of the TIM-3 gene in mice leads to enhanced plaque clearance and improvements in cognitive performance. This finding poses an exciting avenue for intervention—developing a TIM-3 therapy that could ideally inhibit the function of this checkpoint molecule. Subsequently, microglia would regain their phagocytic abilities, clearing the pathological plaques that contribute to neurological decline. Such a therapy holds the potential not only to halt cognitive deterioration in Alzheimer’s patients but also to rejuvenate aspects of memory function that have been lost to the disease.
Mechanisms Behind Microglial Dysfunction
Microglia, the resident immune cells of the central nervous system, play a pivotal role in maintaining brain health by responding to damage and clearing debris. In Alzheimer’s disease, the dysfunction of microglia is largely attributed to heightened levels of TIM-3. When microglia are exposed to amyloid beta, they are meant to engulf and break it down; however, TIM-3 can hamper this process, leading to the accumulation of plaques. This highlights the microglial switch from being protective agents to becoming impeded by their own regulatory mechanisms.
The research indicates that as TIM-3 signaling escalates, the microglia that should normally be engaging with and clearing beta-amyloid plaques instead become inhibited, a phenomenon that can be particularly poignant in older adults suffering from Alzheimer’s. This inability to adequately respond can result in significant cognitive consequences, including memory loss and behavioral changes. Finding ways to reactivate these microglia or counteract TIM-3’s influence could be key in not only Alzheimer’s treatment but potentially in treating other neurodegenerative diseases where plaque accumulation is a hallmark.
The increased expression of TIM-3 on activated microglia is directly correlated with a reduced capacity for clearing plaques from the brain in Alzheimer’s models. Targeting TIM-3 through therapies designed to block this inhibitory pathway could empower microglia to resume their plaque-clearing functions. By alleviating the suppression caused by TIM-3, the therapeutic approach aims to restore the microglial homeostasis that’s critical for managing plaque burden, ultimately leading to improved cognitive outcomes.
Research has begun to pivot towards understanding how immune checkpoint inhibitors can not only be repurposed for cancer treatment but can also offer therapeutic avenues for neurodegenerative disorders. TIM-3 therapy for Alzheimer’s highlights the intersection between cancer immunotherapy strategies and neurobiology, presenting a novel framework for tackling cognitive disorders through modulation of immune checkpoint molecules. The potential parallels between these fields may pave the way for innovative therapies that broaden the scope of existing pharmacological solutions.
Implications for Future Alzheimer’s Treatments
The successful application of TIM-3 therapy in improving cognitive function in mouse models of Alzheimer’s disease presents a promising shift in the therapeutic landscape for this debilitating condition. By targeting the TIM-3 pathway, researchers aim to unlock new potential for reversing cognitive deficits associated with plaque accumulation. Current Alzheimer’s treatments focus primarily on symptomatic relief, but TIM-3 modulation could provide a disease-modifying approach, addressing the underlying mechanisms that contribute to neural decline.
In current research frameworks, trials involving anti-TIM-3 antibodies or small molecules that inhibit TIM-3 will address the critical need to enhance microglial activity against the harmful amyloid deposits in the brain. This approach could lead to paradigm shifts not only in Alzheimer’s treatment but in other neurodegenerative diseases marked by similar immune dysregulations. The coupling of TIM-3 targeting with traditional Alzheimer’s treatments could lead to synergies that boost the efficacy of existing therapies, paving the way for comprehensive multimodal strategies.
Moreover, understanding how TIM-3 functions in the context of Alzheimer’s opens new pathways for potential biomarker development. The presence or levels of TIM-3 in patients may serve as critical indicators of disease progression and treatment efficacy, guiding personalized medicine efforts. As the research progresses, it could lead to new diagnostic tools that facilitate early detection and intervention, improving outcomes for individuals at risk of Alzheimer’s.
Continued collaboration across cognitive neuroscience, immunology, and pharmacology is essential for the successful translation of TIM-3 therapies from bench to clinic. As researchers refine their understanding of TIM-3’s role within the Alzheimer’s pathological landscape, there lies a tremendous opportunity to harness this knowledge in developing effective interventions, ultimately aiming to halt or even reverse the course of Alzheimer’s disease.
Investigating Cognitive Enhancement through TIM-3
Cognitive enhancement through the modulation of TIM-3 pathway presents an intriguing avenue for Alzheimer’s therapeutics. The findings from recent studies suggest that inhibiting TIM-3 in microglia leads to enhanced clearance of amyloid plaques and an overall improvement in cognitive behaviors in mouse models. This advance signifies a potential paradigm shift from focusing solely on symptoms and offers hope for functional recovery in affected individuals. If TIM-3 therapy can be adapted for human use, the implications for enhancing cognition could be substantial.
The cognitive decline associated with Alzheimer’s is frustrating not only for patients but also for caregivers and families. Creating a strategy that leverages TIM-3 inhibition could significantly alter the trajectory of cognition in patients. The ability to restore some level of cognitive function while reducing plaque burden through immunomodulatory strategies such as TIM-3 therapy is a tantalizing possibility. This therapeutic approach aligns with broader goals in Alzheimer’s research, aiming not only for halting the disease’s progression but also for reinvigorating memory faculties that have been compromised.
Furthermore, studies investigating TIM-3 therapy aim to characterize how microglial activity contributes to broader cognitive processes. The enhancement of synaptic plasticity and memory retention, which is influenced by microglial function, is a promising target for future Alzheimer’s treatment strategies. By decreasing TIM-3 activity, researchers hope to unlock pathways that may further promote cognitive enhancement, paving the way for innovative drugs that can genuinely improve the quality of life for those battling Alzheimer’s.
While challenges remain in translating these findings to human models, the possibility of using TIM-3 therapy highlights a novel intersection between immune system modulation and cognitive health. As further research unfolds, exploring the synergistic effects of combining TIM-3 therapy with cognitive training or other pharmacological interventions becomes an avenue to be explored in achieving cognitive enhancement, setting a new standard in Alzheimer’s treatment.
Potential Challenges in Implementing TIM-3 Therapy
While TIM-3 therapy represents a significant advancement in Alzheimer’s research, there are potential challenges that must be addressed before successful implementation in clinical settings. Concerns around specificity and safety in targeting TIM-3 are paramount, especially given its role in regulating immune responses. Therapies that aim to inhibit TIM-3 require careful balancing to avoid unwanted immune activation that could lead to inflammation or autoimmunity, particularly in a context where the brain’s immune regulation is already compromised.
Moreover, the pharmacokinetics of any TIM-3 directed therapeutics need thorough investigation to ensure effective delivery to the brain. As many existing treatments struggle with crossing the blood-brain barrier, ensuring that TIM-3 inhibitors effectively reach their target in the central nervous system without causing neurological side effects will be crucial for their success as treatment options. Consideration of the timing of such therapies in the progression of Alzheimer’s will further dictate their efficacy, necessitating precise clinical trial designs to optimize treatment windows.
Another layer of complexity arises from the genetic diversity among patients, as variations in the TIM-3 gene may present differing responses to therapy. Personalized medicine approaches will be vital in tailoring TIM-3 therapies that account for individual genetic backgrounds and disease pathology. Ongoing research into the multifaceted role of TIM-3 in both cancer and neurodegeneration presents a unique opportunity for collaborative efforts that may enhance our understanding of its inhibition in a therapeutic context.
The upcoming trials evaluating TIM-3 therapy for Alzheimer’s could potentially illuminate these complexities, helping to refine methodologies for safe and effective immunotherapeutic strategies. Such challenges, while daunting, also signify the rigor and potential triumph that may await those who endeavor to navigate the intricate landscape of immune modulation in Alzheimer’s disease.
The Future of Alzheimer’s Treatment: Combining TIM-3 Therapy with Existing Approaches
The future of Alzheimer’s treatment may lie in the integration of TIM-3 therapy with existing strategies, creating a multifaceted approach to combat this complex disease. Recent advancements suggest that targeting immune checkpoints like TIM-3 could synergistically enhance the efficacy of current therapeutic modalities, such as anti-amyloid antibodies. By dismantling the barriers posed by TIM-3 on microglia, researchers envision a dual benefit: improved clearance of amyloid plaques alongside the preservation of neural connections crucial for cognitive function.
Combining TIM-3 therapy with cognitive-enhancing treatments could yield powerful outcomes. As evidence mounts regarding the importance of maintaining a functional immune response in the brain, such combined therapies may enable clinicians to not only halt the progression of Alzheimer’s but also promote recovery in cognitive functions. This holistic approach underscores the necessity for interdisciplinary collaborations, bringing together insights from neurology, immunology, and pharmacology to produce innovative care paradigms tailored to the nuances of Alzheimer’s disease.
Further investigation will be required to determine how best to implement these combinations, particularly regarding dosage, timing, and the specific population of Alzheimer’s patients that are most likely to benefit. Long-term safety and efficacy data will be essential to navigating this new therapeutic landscape. Nevertheless, the prospect of TIM-3 therapy as part of a comprehensive treatment plan represents a hopeful advance in our ongoing fight against Alzheimer’s disease, setting the stage for future discoveries that could transform patient outcomes.
Ultimately, the integration of TIM-3 modulation into existing therapeutic frameworks creates the potential for a new wave of Alzheimer’s therapies aimed not just at managing symptoms but at fundamentally altering the course of the disease. By prioritizing innovative research designs and fostering collaborations across scientific disciplines, we can pave the way for effective interventions that enhance cognitive function and improve quality of life for those affected by Alzheimer’s.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s disease?
TIM-3 therapy for Alzheimer’s disease involves targeting the TIM-3 gene, an immune checkpoint molecule that inhibits microglia from clearing amyloid plaques. Research suggests that blocking TIM-3 can enhance memory and cognition by allowing microglia to effectively eliminate plaque buildup in the brain.
How does TIM-3 influence the microglia’s ability to clear Alzheimer’s plaques?
In Alzheimer’s disease, TIM-3 expression on microglia prevents these immune cells from attacking and clearing amyloid plaques. By inhibiting TIM-3, microglia are activated to engulf and remove plaques, thereby potentially improving cognitive functions and slowing disease progression.
Can TIM-3 therapy improve cognitive function in Alzheimer’s patients?
Research indicates that TIM-3 therapy has the potential to enhance cognitive function in Alzheimer’s models. By deleting or blocking TIM-3, studies have shown improved memory and cognitive behavior in mice, suggesting that similar strategies might benefit Alzheimer’s patients.
What role do immune checkpoint inhibitors like TIM-3 play in Alzheimer’s treatment?
Immune checkpoint inhibitors, such as TIM-3, can modify the behavior of microglia, the brain’s immune cells. In Alzheimer’s treatment, blocking TIM-3 may restore the ability of microglia to target and clear harmful plaques, thus offering a new therapeutic approach to combat cognitive decline.
What potential side effects should be considered with TIM-3 therapy for Alzheimer’s?
While promising, TIM-3 therapy may carry risks associated with activating immune responses. Potential side effects could include inflammation or overreaction of the immune system, which is important to evaluate during clinical trials.
How does the TIM-3 gene relate to late-onset Alzheimer’s disease?
The TIM-3 gene, specifically the HAVCR2 polymorphism, is linked to late-onset Alzheimer’s disease. Variants of this gene can affect the expression of TIM-3 on microglia, hence playing a role in the disease’s pathology and potential treatment strategies.
What is the significance of the research conducted on TIM-3 therapy for Alzheimer’s?
The research on TIM-3 therapy highlights a novel approach that could lead to effective Alzheimer’s treatments by reactivating microglia to clear amyloid plaques. This strategy is especially significant given the previous challenges in developing successful Alzheimer’s medications.
When will TIM-3 therapy for Alzheimer’s disease be available for humans?
Currently, researchers are conducting preclinical trials using mouse models that express the human TIM-3 gene. The timeline for human trials and availability of TIM-3 therapy in clinical settings will depend on the outcomes of these studies and subsequent regulatory approvals.
| Key Points |
|---|
| Recent study indicates TIM-3 therapy may help Alzheimer’s patients by enhancing microglial activity to clear amyloid plaques. |
| 90-95% of Alzheimer’s cases are late-onset and linked to the TIM-3 molecule as a genetic risk factor. |
| TIM-3 acts as a checkpoint molecule, inhibiting microglial action to clear plaque in the brain. |
| Research showed that deleting TIM-3 in mice improved plaque clearance and cognitive behavior. |
| Possible therapeutic applications include anti-TIM-3 antibodies to enhance microglial response against plaques. |
| Ongoing studies aim to test human anti-TIM-3 antibodies in humanized mouse models of Alzheimer’s. |
Summary
TIM-3 therapy for Alzheimer’s shows promise as a groundbreaking approach that leverages the immune system to address a critical challenge in combating the disease. By inhibiting the TIM-3 checkpoint molecule, researchers have uncovered a method to enable microglial cells to effectively target and clear harmful amyloid plaques from the brain, significantly improving cognitive function in mouse models. As scientists explore the potential of translating these findings into clinical therapies, TIM-3 therapy for Alzheimer’s may represent a significant advance in the pursuit of effective treatments for this debilitating disease.